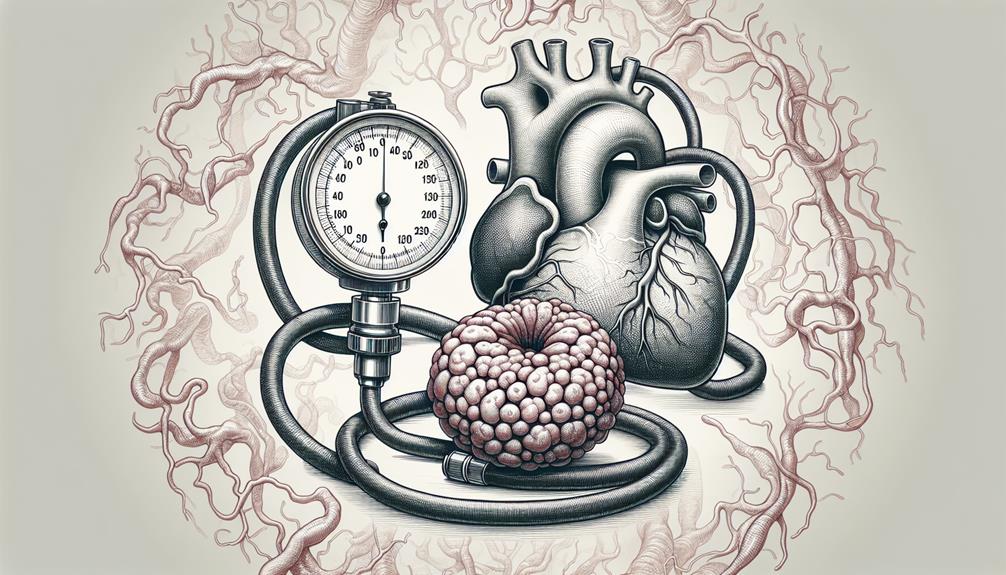
As you explore the complexities of hyperthyroidism and its effects on blood pressure, you'll find that grasping the mechanics of thyroid hormones and their influence on your cardiovascular system is key. When your thyroid overproduces these hormones, it's not just your metabolism that's affected; your heart rate and vascular resistance are, too, potentially leading to heightened blood pressure. Effective management hinges on a nuanced understanding of these dynamics. This might leave you wondering how exactly these elements interact and what strategies can best mitigate the associated risks, setting the stage for a deeper examination of the potential implications for your health.
Overview of Hyperthyroidism and Hypertension
You've likely heard of hyperthyroidism, a condition marked by an overactive thyroid gland accelerating your body's metabolism, which can also impact your blood pressure.
Understanding how this thyroid dysfunction can lead to hypertension requires a clear look at both the diagnostic criteria and treatment options available for hyperthyroidism.
Analyzing this relationship further, it's essential to explore how elevated thyroid hormones potentially elevate arterial pressure, intensifying the risk of hypertension.
Hyperthyroidism
You need to understand that hyperthyroidism, characterized by an overactive thyroid gland, greatly influences systemic blood pressure. Key causes include Graves' disease, toxic adenoma, and subacute thyroiditis, each leading to an excess of thyroid hormones that can accelerate your heart rate and disrupt normal blood pressure regulation.
Recognizing symptoms such as weight loss, increased heart rate, and anxiety is essential for timely diagnosis and management.
Causes and Symptoms of Hyperthyroidism
Several factors can cause hyperthyroidism, a condition characterized by the overproduction of thyroid hormones, which greatly impacts metabolic rates and cardiovascular health.
You'll find that autoimmune disorders like Graves' disease are primary culprits. Symptoms often include unexpected weight loss, rapid heartbeat, increased appetite, and nervousness.
These manifestations result from your thyroid gland's excessive hormone production, which accelerates your body's metabolic processes.
Diagnosis and Treatment Options for Hyperthyroidism
Doctors typically diagnose hyperthyroidism through blood tests that measure thyroid hormone levels and assess symptoms to determine the appropriate treatment options. The main tests include the TSH (Thyroid-Stimulating Hormone) assay, Free T4, and Free T3. Low TSH levels often indicate an overactive thyroid, especially when accompanied by high levels of T4 and T3.
Once you're diagnosed, treatment options vary based on the severity of your condition and your overall health. Antithyroid medications, such as methimazole or propylthiouracil, are often the first line of treatment. These drugs work by inhibiting your thyroid's ability to produce hormones. However, it's essential to monitor liver function and white blood cell counts regularly, as these medications can cause adverse effects.
Another option is radioactive iodine therapy, which involves taking a radioactive iodine capsule or liquid that destroys thyroid cells, reducing hormone production. This treatment may lead to hypothyroidism, necessitating lifelong thyroid hormone replacement therapy.
Surgical removal of the thyroid (thyroidectomy) might be necessary if other treatments are ineffective or if you have a large goiter causing physical discomfort or breathing difficulties. Post-surgery, you'll likely need thyroid hormone replacement therapy to maintain normal hormone levels.
Your doctor will guide you through these options, considering your specific medical circumstances to find the most effective treatment.
Exploring Hypertension
As you explore the relationship between hyperthyroidism and blood pressure, it's essential to understand hypertension's basics.
Hypertension, characterized by persistently high blood pressure, poses significant health risks if left unmanaged.
Definition and Risk Factors of Hypertension
What exactly is hypertension, and what factors increase your risk of developing this condition?
Hypertension, or high blood pressure, occurs when your blood pressure levels consistently exceed normal ranges.
Risk factors include obesity, a sedentary lifestyle, excessive salt intake, aging, genetic predisposition, and chronic conditions such as diabetes or kidney disease.
Understanding these can help you mitigate risks through targeted lifestyle changes and medical interventions.
Relation Between Hyperthyroidism and Hypertension
Understanding the relationship between hyperthyroidism and hypertension is imperative, as the former can greatly influence the development and management of high blood pressure. Hyperthyroidism accelerates your body's metabolism, signaling your heart to pump harder and faster, which raises blood pressure levels. It's vital to grasp how thyroid hormones interact with vascular resistance and cardiac output.
Firstly, the excess of thyroid hormones typically found in hyperthyroidism increases heart rate and forces the heart to work more vigorously, thereby elevating systolic and diastolic blood pressure. This state of increased cardiac output can lead to systolic hypertension.
Additionally, thyroid hormones directly affect the smooth muscle cells in your arterial walls, causing them to relax and decrease systemic vascular resistance. However, this reduction isn't enough to offset the rise in blood pressure caused by increased cardiac output.
Moreover, you'll find that hyperthyroidism impacts renal function, enhancing sodium reabsorption which contributes to volume expansion, further exacerbating hypertension. Managing hyperthyroidism, thus, involves careful monitoring and control of thyroid hormone levels to mitigate these effects on blood pressure.
Impact of Hyperthyroidism on Blood Pressure
You'll find that hyperthyroidism can greatly influence your blood pressure, primarily through mechanisms that increase your heart rate and reduce vascular resistance.
Understanding these mechanisms is essential for devising effective management strategies to control hypertension in affected patients.
Mechanisms of Hyperthyroidism-Induced Hypertension
Hyperthyroidism raises blood pressure through several mechanisms, including increased heart rate and enhanced sensitivity of blood vessels to catecholamines. When your thyroid gland produces too much thyroid hormone, it accelerates your body's metabolism, leading to an increase in your heart rate and a higher cardiac output. This is the volume of blood your heart pumps in a minute, and its increase places additional load on your blood vessels.
Moreover, the excess thyroid hormones make your blood vessels more responsive to catecholamines such as adrenaline and noradrenaline. These hormones typically cause vasoconstriction, or the narrowing of blood vessels, which increases blood pressure. In hyperthyroidism, this response is exaggerated, further elevating your blood pressure levels.
The thyroid hormones also affect the renin-angiotensin-aldosterone system (RAAS), which regulates blood pressure and fluid balance. Increased thyroid hormone levels lead to enhanced renin release from the kidneys, which in turn increases angiotensin II and aldosterone levels, contributing to hypertension by promoting water and sodium retention and further vasoconstriction.
Understanding these mechanisms is important because it highlights the direct impact hyperthyroidism can have on your cardiovascular system, emphasizing the need for careful monitoring and management of thyroid function to maintain blood pressure within a healthy range.
Management Strategies for Controlling Blood Pressure in Hyperthyroid Patients
You'll find that managing your blood pressure if you have hyperthyroidism involves a combination of medication and lifestyle adjustments.
Beta-blockers are often prescribed to decrease your heart rate and reduce blood pressure, while changes in diet and exercise can further help stabilize your cardiovascular system.
It's essential to monitor these interventions closely, as they directly influence the effectiveness of your overall treatment plan for hyperthyroidism.
Role of Medications and Lifestyle Changes
Effective management of blood pressure in hyperthyroid patients often involves a combination of targeted medications and strategic lifestyle adjustments.
- Beta-blockers: Visualize them calming your racing heart, easing the burden on your cardiovascular system.
- Salt restriction: Imagine your meals with less salt, reducing fluid retention and lowering blood pressure.
- Regular exercise: Picture a structured routine strengthening your heart and enhancing blood flow.
Research Studies on Hyperthyroidism and Blood Pressure
As you explore research studies on hyperthyroidism and blood pressure, you'll find that a meticulous analysis of scholarly articles reveals significant correlations.
Reviewing hypertension literature, researchers consistently link thyroid dysfunction to altered hemodynamic states.
Recent findings in this field emphasize the need for a nuanced understanding of how thyroid activity influences blood pressure regulation.
Analysis of Hyperthyroidism Scholarly Articles
Recent studies have shown a complex assemblage between hyperthyroidism and elevated blood pressure, necessitating a deeper examination of the underlying mechanisms and implications for treatment. As you explore the current scholarly articles, you'll find a robust discussion on how excess thyroid hormones play a pivotal role in cardiovascular function.
The surge in thyroid hormones typically seen in hyperthyroidism can lead to an increase in heart rate and overall cardiac output, which often precipitates a rise in systolic blood pressure.
In your investigation, you'll encounter several key themes:
- The Role of Thyroid Hormones: These studies frequently measure the levels of T3 and T4 hormones and their direct effects on vascular resistance and arterial stiffness.
- Genetic Predispositions and Environmental Factors: Research elucidates how genetics and lifestyle choices compound the risk and severity of hypertension in hyperthyroid patients.
- Treatment Efficacy and Outcomes: A critical analysis of various treatment modalities, from antithyroid medications to beta-blockers, and their differential impacts on managing blood pressure in affected individuals.
Understanding these elements is important. You'll see that managing hyperthyroidism isn't just about normalizing thyroid hormone levels; it's also about mitigating associated cardiovascular risks, including hypertension.
Reviewing Hypertension Scholarly Articles
You'll discover that scholarly articles on hypertension in hyperthyroid patients often highlight the critical interplay between thyroid function and cardiovascular health. These studies underscore how excess thyroid hormones can escalate heart rate and contractility, which in turn can lead to elevated blood pressure levels. This connection is essential for understanding the broader impact of thyroid disorders on overall cardiovascular risk.
Diving deeper, you'll find that research typically focuses on the mechanisms through which thyroid hormones influence vascular resistance and cardiac output. For instance, thyroxine (T4) and triiodothyronine (T3), the principal hormones produced by the thyroid gland, are found to enhance the responsiveness of vascular smooth muscle to catecholamines, thereby increasing cardiac output.
Additionally, hyperthyroidism is associated with a reduction in systemic vascular resistance, which can initially lead to a decrease in diastolic blood pressure but an increase in systolic pressure, creating a wider pulse pressure.
Analyses of these dynamics are critical for clinicians who manage patients with coexistent thyroid and cardiovascular conditions. Understanding these pathways helps in tailoring treatment strategies that address both the thyroid condition and its cardiovascular manifestations, ensuring a holistic approach to patient care.
Recent Findings in Blood Pressure Articles
Researchers have uncovered noteworthy connections between hyperthyroidism and elevated systolic blood pressure, revealing intricate interactions that impact cardiovascular health.
As you explore the recent studies, you'll discover that the excess thyroid hormone increases heart rate and cardiac output, which can greatly escalate your systolic blood pressure. This isn't just a simple elevation; it's a dynamic alteration that could predispose you to other cardio risks.
Consider these specific areas from the latest research:
- Thyroid Function and Vascular Stiffness: Enhanced thyroid activity is associated with a decrease in arterial compliance, which means your arteries can't expand as freely. This rigidity forces your heart to pump harder, raising systolic pressure.
- Endothelial Function Deterioration: Hyperthyroidism disrupts the endothelium, the lining of your blood vessels, impairing its ability to regulate vascular tone and blood flow, further contributing to hypertension.
- Autonomic Nervous System Imbalance: Excessive thyroid hormones can overstimulate your sympathetic nervous system, leading to increased blood pressure levels. This imbalance not only elevates your systolic pressure but also poses a risk for arrhythmias.
These findings underscore the importance of monitoring thyroid levels as part of your cardiovascular risk management strategy.
If you're exploring these aspects, understanding these mechanisms can be pivotal in optimizing your treatment plan.