When Sarah, a 28-year-old graphic designer, was unexpectedly diagnosed with aplastic anemia, it highlighted the vital importance of being informed about this rare condition. You might not think it’s necessary to know the ins and outs of such a specific medical issue unless you’re directly affected, but understanding aplastic anemia can greatly impact the quality of care and support patients like Sarah receive. With advances in treatment and diagnosis continually evolving, staying abreast of the latest research isn’t just beneficial; it’s essential. Now, consider the implications for patients who might be silently struggling without a correct diagnosis. What if you or someone close to you were in their shoes?
Overview of Aplastic Anemia
Aplastic anemia is characterized by the failure of your bone marrow to produce sufficient blood cells, encompassing several types, each with distinct etiologies.
You’ll find that its pathophysiology often involves immune system dysfunction, which mistakenly targets hematopoietic cells, leading to pancytopenia.
Accurate diagnosis hinges on recognizing clinical manifestations which differ from other hematologic disorders, supported by specific laboratory findings.
Definition and Types of Aplastic Anemia
Aplastic anemia is a rare but serious condition that results from the failure of your bone marrow to produce adequate blood cells.
Its incidence varies, with certain genetic, environmental, and medical factors elevating risk.
Understanding these epidemiological trends and associated risk factors is essential for effective diagnosis and management.
Epidemiology and Risk Factors
Understanding the distribution and factors that increase the likelihood of developing aplastic anemia is essential for both patients and healthcare providers. Globally, incidence varies, with higher rates in East Asia.
You’re at increased risk if exposed to radiation, certain chemicals, or use specific drugs. Genetic predispositions also play a critical role. Accurate epidemiological data supports targeted prevention strategies and optimizes therapeutic approaches.
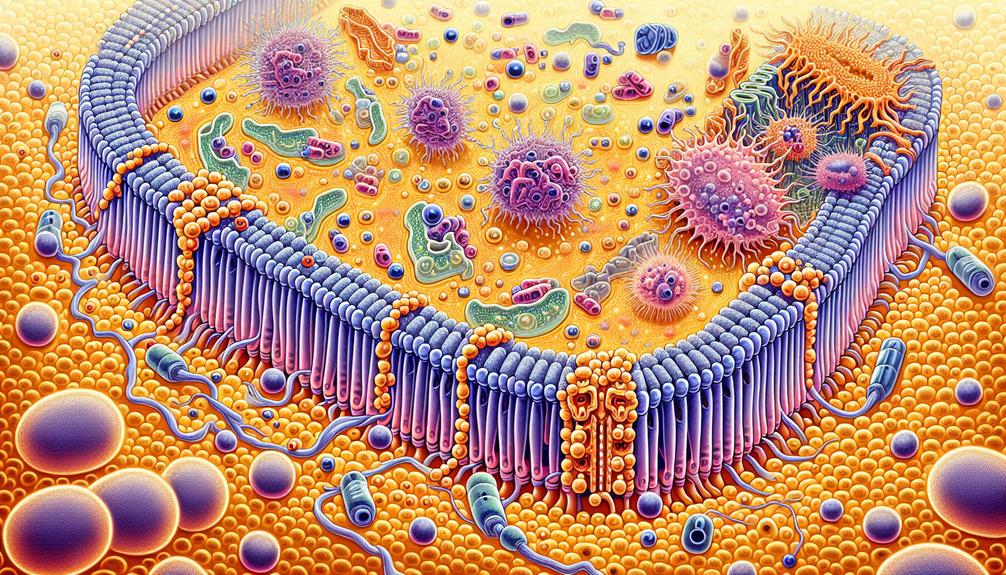
Pathophysiology of Aplastic Anemia
In aplastic anemia, you’re dealing with a critical failure of your bone marrow‘s ability to produce blood cells, a condition rooted in stem cell deficiency.
Research indicates that this failure often stems from an autoimmune attack on your hematopoietic cells, disrupting the essential cell production.
Understanding the molecular pathways behind this attack provides insight into potential therapeutic targets and management strategies.
Bone Marrow Failure Mechanism
At the heart of aplastic anemia, your bone marrow ceases to produce sufficient new blood cells, leading to multiple systemic failures.
This failure stems from damage to hematopoietic stem cells, essential for generating blood components. Factors include autoimmune attacks, exposure to toxins or radiation, and genetic predispositions.
Consequently, you’re left vulnerable to infections, anemia, and bleeding complications, underscoring the condition’s severity and complexity.
Immune System Dysfunction
Your immune system plays a vital role in the development of aplastic anemia, often mistakenly attacking the bone marrow’s stem cells. This autoimmune attack leads to a deficiency in the production of new blood cells, a condition termed as pancytopenia.
Research indicates that T-cells, a type of lymphocyte responsible for cell-mediated immunity, are often implicated in this pathogenic process. They’re known to become autoreactive and target hematopoietic stem cells, the precursors to all blood cell types.
The mechanistic pathways involve the activation of various cytokines, including interferon-gamma and tumor necrosis factor-alpha, which have been observed to inhibit hematopoiesis. This cytokine milieu creates an environment hostile to stem cell growth, leading to their destruction or dysfunction.
Additionally, the expression of antigens like HLA-DR on these stem cells can exacerbate their vulnerability to T-cell mediated cytotoxicity.
Understanding these immunological underpinnings is important, as they not only elucidate the etiology of aplastic anemia but also guide therapeutic interventions.
Immunosuppressive therapies, such as antithymocyte globulin and cyclosporine, target these aberrant immune responses, aiming to halt the progression of the disease and restore normal hematopoiesis.
Diagnosis and Clinical Manifestations
You may first notice symptoms like fatigue, bruising, or frequent infections, indicating a possible case of aplastic anemia.
Diagnostic confirmation involves specific blood tests including a complete blood count (CBC), which typically shows pancytopenia, and a bone marrow biopsy to assess the cellularity of your marrow.
These tests are critical in distinguishing aplastic anemia from other hematologic disorders and determining the severity of the condition.
Symptoms and Diagnostic Tests
Recognizing the symptoms of aplastic anemia and undergoing the appropriate diagnostic tests are critical steps in accurately identifying this potentially life-threatening condition.
- Persistent Fatigue: Picture the unyielding exhaustion, no matter the amount of rest.
- Pale Skin: Visualize a noticeable loss of color, a ghostly pallor.
- Frequent Infections: Imagine battling back-to-back illnesses, a relentless cycle.
- Easy Bruising: Envision bruises appearing from minor bumps.
- Nosebleeds: Think of unexpected, sudden bleeding without apparent cause.
Differential Diagnosis
When evaluating a patient suspected of having aplastic anemia, it’s vital to differentiate this condition from other hematologic disorders that can present with similar symptoms. Aplastic anemia, characterized by pancytopenia and a hypocellular bone marrow, must be distinguished from other causes of bone marrow failure such as myelodysplastic syndromes (MDS), paroxysmal nocturnal hemoglobinuria (PNH), and large granular lymphocyte (LGL) leukemia.
You’ll find that distinguishing aplastic anemia from MDS is important, as MDS often presents with dysplastic changes in the marrow, which are typically absent in aplastic anemia. A bone marrow biopsy is instrumental in this evaluation, providing clear evidence of the marrow’s cellularity and the presence of dysplastic features.
Similarly, differentiating aplastic anemia from PNH involves testing for the presence of GPI-anchored protein-deficient cells using flow cytometry, which is positive in PNH but not in aplastic anemia. Also, consider LGL leukemia, which can mimic aplastic anemia but usually exhibits an abnormal population of large granular lymphocytes in the blood or marrow.
Accurate diagnosis is critical, as it directly influences the management strategy and prognosis. Therefore, a detailed clinical evaluation, corroborated by specific laboratory tests and bone marrow examination, is indispensable in the differential diagnosis of aplastic anemia.
Treatment Approaches for Aplastic Anemia
When addressing aplastic anemia, you’ll find that immunosuppressive therapy is a cornerstone of treatment, especially for those who aren’t suitable candidates for stem cell transplantation.
This approach involves the administration of medications such as antithymocyte globulin and cyclosporine, which effectively suppress the immune system’s activity that’s responsible for damaging bone marrow.
Clinical trials have demonstrated that this method can lead to hematologic improvement and reduced need for transfusions in many patients.
Immunosuppressive Therapy
Immunosuppressive therapy effectively treats aplastic anemia by suppressing the immune system’s abnormal response that damages bone marrow.
*Syringes and vials of medication* illustrate the administration of treatment.
*White blood cells under a microscope* depict the target of the therapy.
*A serene patient receiving treatment* emphasizes hope and recovery.
*Detailed medical charts* track progress and response to therapy.
*A calm, clinical setting* conveys a controlled and professional therapeutic environment.
Hematopoietic Stem Cell Transplantation
Hematopoietic stem cell transplantation offers a potentially curative treatment for patients with severe aplastic anemia. This procedure involves the infusion of stem cells from a compatible donor, usually a sibling, to restore your bone marrow’s ability to produce blood cells. It’s important that you’re matched closely with a donor to minimize risks and enhance the success rate of the transplant.
The process starts with conditioning, where you’ll receive chemotherapy and sometimes radiation to eradicate your diseased marrow. This makes room for the donor’s healthy cells to engraft. Post-transplant, you’ll undergo immunosuppression to prevent graft-versus-host disease (GVHD), a condition where the donor cells attack your body.
Success rates vary, influenced by factors such as donor match quality, your age, and the condition of your health prior to the transplant. Younger patients typically have higher success rates, with studies showing improved long-term survival rates for those under 20.
It’s also essential to have regular follow-ups to monitor for complications like infections and organs’ function, which are critical in the first few months post-transplant. Understanding these aspects can help you weigh the benefits against the potential risks involved in undergoing hematopoietic stem cell transplantation for aplastic anemia.
Prognosis and Complications
You’ll find that the long-term outlook and survival rates for aplastic anemia vary greatly, influenced by factors such as age, severity of the condition, and treatment response.
Studies indicate that with prompt and appropriate treatment, survival rates can improve substantially, particularly in younger patients or those who undergo stem cell transplantation.
However, untreated or severe cases can lead to serious complications, including life-threatening infections and bleeding.
Long-Term Outlook and Survival Rates
The long-term outlook for patients with aplastic anemia greatly depends on timely diagnosis and appropriate treatment strategies.
- *Bone marrow transplant* success rates are improving annually.
- *Immunosuppressive therapies* notably extend survival.
- *Regular monitoring* helps prevent severe complications.
- *Advancements in genetic testing* continue to refine treatment options.
- *Supportive care improvements* significantly enhance the quality of life.
Complications and Management Strategies
Managing aplastic anemia involves addressing its severe complications, such as infections and bleeding, which require prompt and precise medical interventions. As your bone marrow fails to produce adequate blood cells, you’re particularly susceptible to bacterial and fungal infections due to neutropenia, a notable decrease in neutrophils that are essential for fighting pathogens. Prophylactic antibiotic, antiviral, and antifungal therapies are often employed to prevent such infections.
Bleeding complications arise from thrombocytopenia, where the platelet count is dangerously low. You’ll need regular platelet transfusions to maintain a safer platelet count and avoid serious bleeding episodes. Additionally, the use of agents like antifibrinolytics can help stabilize clot formation, reducing the risk of hemorrhage.
Hemoglobin levels are crucially monitored, and erythrocyte transfusions might be necessary to treat symptomatic anemia, aiming to maintain hemoglobin above certain clinically significant thresholds to guarantee adequate oxygenation of tissues.
Immunosuppressive therapy, including agents like antithymocyte globulin and cyclosporine, is pivotal in treating aplastic anemia by suppressing the immune system’s attack on your bone marrow. Additionally, bone marrow transplantation from a compatible donor might be considered, especially if you don’t respond to other treatments. This approach requires careful donor selection and post-transplant care to minimize graft-versus-host disease and other complications.
Current Research and Future Directions
You’ll find that recent advances in aplastic anemia research have ushered in a range of innovative therapies, now being tested in clinical trials.
These trials are critical as they assess both the efficacy and safety of potential new treatments that could significantly alter standard care practices.
It’s essential to monitor these developments to understand how they might improve outcomes for patients diagnosed with this challenging condition.
Innovative Therapies and Clinical Trials
Researchers are currently exploring several groundbreaking therapies and conducting clinical trials to better understand and treat aplastic anemia.
- Gene Therapy: Targeting genetic mutations responsible for bone marrow failure.
- Immunosuppressive Treatments: Enhancing patient-specific immune modulation.
- Stem Cell Enhancements: Innovating transplantation techniques.
- Biological Agents: Developing new biologic drugs.
- Precision Medicine: Tailoring treatments based on individual genetic profiles.
Challenges in Aplastic Anemia Research
Several formidable challenges confront the advancement of research in aplastic anemia, a complex bone marrow failure disorder. First, the rarity of the disease poses a substantial obstacle to large-scale studies, making it difficult to gather sufficient data for robust statistical analysis. This scarcity of patients often results in underpowered studies that may fail to detect significant effects of potential treatments.
Additionally, the etiology of aplastic anemia is multifaceted, involving both genetic predispositions and environmental factors. Disentangling these elements requires sophisticated, multidisciplinary approaches and technologies, such as genome-wide association studies (GWAS) and next-generation sequencing, which are resource-intensive and require specialized expertise.
You’re also facing challenges in the standardization of treatment protocols. With the disease manifesting differently across patients, individualized treatment approaches are necessary, complicating the establishment of standardized treatment guidelines that are critical for comparative studies and the development of new therapies.
Conclusion
Understanding aplastic anemia‘s complexities and treatment options empowers you to make informed health decisions. This condition, characterized by the failure of bone marrow to produce sufficient blood cells, necessitates a nuanced understanding of both its pathophysiology and the therapeutic avenues available.
As you navigate this landscape, consider the critical role of evidence-based knowledge in managing your health or supporting others.
Visualize the following to grasp the impact and necessary interventions for aplastic anemia:
- *A microscope slide revealing scanty bone marrow cells*, contrasted with a healthy sample bustling with activity.
- *A calendar marked with regular clinic visits*, symbolizing the ongoing monitoring required in disease management.
- *A vibrant graph displaying blood cell counts*, illustrating the fluctuations that guide treatment adjustments.
- *A serene image of a supportive group*, representing the psychological and communal support that’s crucial.
- *A detailed chart of medication regimens*, with annotations for dosages and side effects, highlighting the tailored approach in treatment.
Each image underscores the importance of staying informed and proactive about this rare but manageable condition. With the right knowledge, you can effectively advocate for excellent care and outcomes.