When the FDA approved hydroxyurea in 1998 for the treatment of sickle cell anemia, it marked a significant milestone in the battle against this debilitating disease. As you explore this guide, you’ll gain insights into how such advancements have paved the way for newer therapies and research methodologies. You’ll find discussions on the intricacies of gene therapy, challenges in healthcare delivery, and the promise of emerging technologies. This guide doesn’t just recount historical breakthroughs; it connects you with the current dialogue among experts and points towards the untapped potential that could dramatically alter the landscape of sickle cell disease management. What might the next big breakthrough be?
Sickle Cell Anemia
As you explore the complexities of sickle cell anemia, you’ll find that understanding its basics is essential for grasping how symptoms and complications develop.
You’ll examine the epidemiology and global impact, noting variations in prevalence and the challenges these pose to healthcare systems worldwide.
Moreover, you’ll assess the challenges in treatment and management, recognizing the hurdles in achieving effective patient care.
the Basics of Sickle Cell Anemia
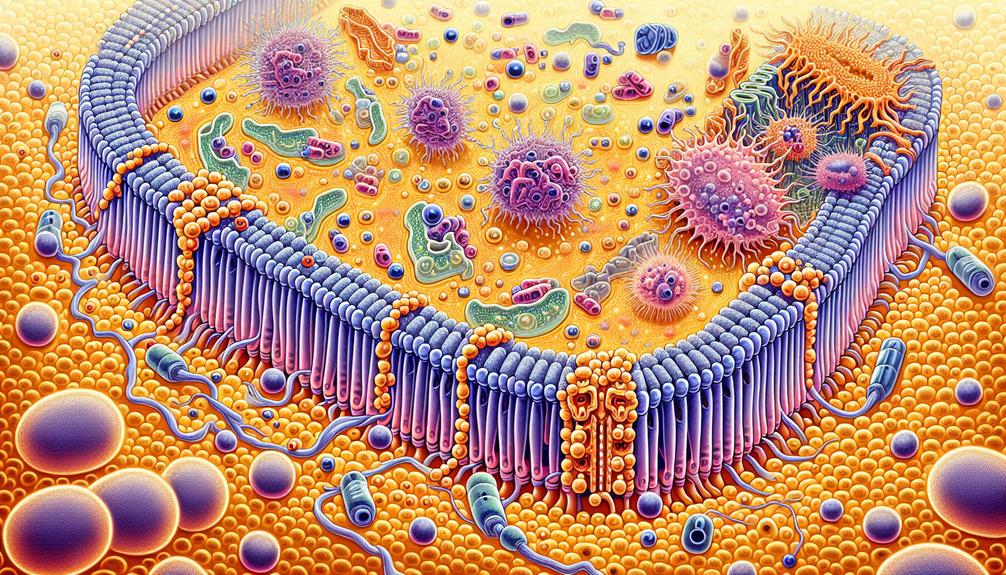
You must understand that sickle cell anemia is primarily caused by a genetic mutation which leads to the production of hemoglobin S, rather than the normal hemoglobin A.
This abnormal hemoglobin causes red blood cells to distort into a sickle shape, severely impacting their functionality and life span.
This mutation’s inheritance follows an autosomal recessive pattern, where two copies of the mutated gene are required for the full-blown disease manifestation.
Genetic Mutation and Hemoglobin S
Understanding the genetic mutation responsible for sickle cell anemia reveals how normal hemoglobin A morphs into hemoglobin S, a variant that dramatically alters red blood cell function.
This mutation occurs in the HBB gene, specifically a single nucleotide change that causes glutamic acid to be replaced by valine.
This substitution distorts hemoglobin’s structure, promoting the sickling of red cells, which impedes blood flow and causes severe clinical symptoms.
Symptoms and Complications
Many individuals with sickle cell anemia experience a range of symptoms and complications that greatly impact their daily lives.
You might notice that the hallmark symptom, vaso-occlusive pain, arises from misshapen, rigid red blood cells obstructing blood flow. This painful event, often called a ‘sickle cell crisis,’ can last from hours to days, causing severe discomfort and necessitating medical intervention.
Additionally, you’re at an increased risk of infections due to spleen damage. The spleen helps filter bacteria from your blood, but sickled cells can impair this function. Consequently, you might find yourself more susceptible to bacterial infections, which can be potentially life-threatening without prompt treatment.
Chronic anemia is another concern. The irregularly shaped red blood cells have a shortened lifespan, leading to a persistent shortage that can cause fatigue, weakness, and an increased heart rate. This chronic depletion can reduce your quality of life and limit your daily activities.
You should also be aware of potential organ damage over time. Organs that don’t receive adequate blood flow can suffer from episodes of acute pain and long-term dysfunction. Regular monitoring and management are essential to mitigate these risks and preserve organ function as much as possible.
Epidemiology and Global Impact
As you examine the epidemiology of sickle cell anemia, consider the varying prevalence rates across different regions, reflecting genetic, environmental, and social factors.
You’ll find that sub-Saharan Africa, parts of the Mediterranean, and the Middle East report the highest incidence due to the protective trait against malaria linked to the sickle cell gene.
Analyzing these patterns provides essential insights into the global impact and challenges in managing this hereditary disease.
Prevalence in Different Regions
Sickle cell anemia’s prevalence varies markedly across different regions, reflecting patterns of genetic adaptation to historical malaria exposure.
Sub-Saharan Africa: Rates soar up to 2%, correlating with malaria’s stronghold.
Middle East and India: Moderate prevalence, around 1-1.5%, due to similar historical malaria pressures.
United States and Europe: Lower prevalence, generally below 0.1%, with cases primarily among African descent populations.
Challenges in Treatment and Management
Patients with sickle cell anemia face numerous treatment challenges, including managing pain crises and preventing infections. You’ll find that the irregularly shaped red blood cells in your bloodstream, which characterize this genetic disorder, often lead to vaso-occlusive crises. These painful episodes can be unpredictable and severe, requiring acute management strategies that range from hydration to opioid administration for pain relief. However, the chronic use of opioids poses its own risks, such as dependency and decreased efficacy over time.
Moreover, your susceptibility to infections is markedly increased due to spleen dysfunction, often necessitating regular vaccinations and prophylactic antibiotics. Yet, these measures aren’t foolproof; breakthrough infections can still occur, compounding your health challenges.
Long-term treatment strategies also include disease-modifying therapies such as hydroxyurea, which can reduce the frequency of pain crises and acute chest syndrome incidents. It’s important, however, to monitor for potential side effects, including myelosuppression and increased risk of malignancies. Advances in gene therapy and bone marrow transplants offer hope but are limited by high costs and the need for suitable donor matches, making widespread application challenging.
Navigating these treatment landscapes requires a collaborative approach involving specialized healthcare providers to tailor interventions that maximize efficacy while minimizing adverse effects.
Advancements in Sickle Cell Anemia Research
You’ll find that recent advancements in sickle cell anemia research have greatly broadened treatment horizons.
Innovations in genetic therapy focus on precise genetic modifications to ameliorate disease symptoms, while studies in stem cell transplantation are evaluating its efficacy as a curative approach.
Concurrently, ongoing drug development and clinical trials aim to enhance pain management and quality of life, with careful attention to patient recruitment and ethical standards.
Genetic Therapy Innovations
You’ve likely heard of CRISPR-Cas9, a groundbreaking gene-editing tool that’s reshaping how we approach genetic disorders, including sickle cell anemia.
This technology allows scientists to precisely target and modify DNA sequences, potentially correcting the genetic mutations at the root of this debilitating disease.
Its application in clinical trials has shown promising results, offering a potential pathway to not just manage but cure sickle cell anemia.
CRISPR-Cas9 and Gene Editing Techniques
CRISPR-Cas9, a revolutionary gene-editing technology, has ushered in significant advancements in the treatment of sickle cell anemia by enabling precise alterations to the genetic code.
Here’s why it’s a game-changer:
- Targeted Correction: Allows direct modification of the HBB gene mutations responsible for sickle cell disease.
- Permanent Solutions: Potentially offers a one-time, curative treatment.
- Reduced Complications: Aims to decrease the associated clinical complications considerably.
Stem Cell Transplantation Studies
Recent advancements in stem cell transplantation offer promising outcomes for those battling sickle cell anemia, highlighting significant improvements in both safety and efficacy.
As you explore the latest studies, it’s important to understand that stem cell transplantation involves replacing the diseased bone marrow of a patient with healthy stem cells, aiming to produce normal red blood cells. This method has transcended traditional boundaries through the development of reduced-intensity conditioning (RIC) regimens which make the procedure accessible to a broader range of patients by minimizing the risk of complications commonly associated with conventional transplantation methods.
Moreover, the utilization of matched sibling donors has enriched the success rates of engraftment and reduced the incidence of graft-versus-host disease, a serious and potentially fatal complication. However, the challenge remains in finding suitable donors for a large percentage of patients, which underscores the importance of ongoing research in haploidentical transplants and cord blood transplants as viable alternatives.
Your understanding of these advancements should include a recognition of the meticulous patient selection and pre-transplant conditioning that are critical to enhancing patient outcomes. As researchers continue to refine these protocols, your insight into this field will expand, opening up new vistas for both treatment and eventual cure.
Drug Development and Clinical Trials
You’ve observed the landscape of drug development constantly evolving in response to the complexities of sickle cell anemia.
Current medications offer limited relief, primarily targeting symptom management rather than the underlying genetic anomalies.
Future prospects in clinical trials are geared toward innovative therapies that aim to modify gene expression and enhance the quality of life for patients.
Current Medications and Future Prospects
Advancements in drug development and clinical trials are greatly improving treatment options for sickle cell anemia.
- Hydroxyurea: Enhances fetal hemoglobin production, reducing painful episodes.
- Crizanlizumab: Recently approved, this drug prevents painful crises by blocking selectin, which causes cell adhesion.
- Gene Therapy: Promising results in trials, potentially offering a cure by correcting the gene defect responsible for the disease.
Patient Recruitment and Ethical Considerations
In recruiting patients for sickle cell anemia studies, researchers must rigorously adhere to ethical standards to guarantee informed consent and protect participant welfare. You’re at the center of crafting a research environment that respects and safeguards the rights of study participants.
It’s imperative you confirm all potential recruits fully understand the study’s scope, including any risks and benefits, through a clear and detailed informed consent process. This isn’t just a formality; it’s a fundamental right of the participants.
As you devise recruitment strategies, you must also ensure that they’re fair and non-coercive. This involves developing a protocol that allows for the inclusion of a diverse patient population, reflecting the genetic variability within the sickle cell disease spectrum.
You’ll need to be particularly vigilant about avoiding any form of undue inducement that might influence a participant’s decision to join a study.
Impact of Sickle Cell Anemia Studies on Patient Care
You’ll find that recent studies on sickle cell anemia have greatly enhanced patient care by focusing on improving life quality through innovative treatments and holistic support systems.
These studies underline the necessity for tailored psychosocial support and rigorous patient education programs to manage the complexities of the disease.
Additionally, they advocate for improved healthcare policies and equitable access to treatments, ensuring that all patients receive the care they deserve.
Improving Quality of Life through Research
You’ll find that recent advancements in pain management strategies for sickle cell anemia have greatly altered patient care protocols. These strategies focus on both pharmacologic interventions, such as the optimized use of opioids and adjuvant therapies, and non-pharmacologic approaches, including cognitive behavioral therapy and physical rehabilitation.
These holistic approaches not only aim to reduce the frequency and severity of pain episodes but also enhance your overall functional capacity and quality of life.
Pain Management Strategies
Research into pain management strategies offers crucial insights that directly enhance the care and quality of life for patients suffering from sickle cell anemia.
Here are three key strategies:
- Optimized Opioid Use: Carefully balancing efficacy and dependency risks.
- Adjuvant Therapies: Incorporating anti-inflammatory drugs to reduce episodic pain severity.
- Patient Education: Empowering you with knowledge to effectively manage pain crises.
Psychosocial Support and Patient Education
Understanding psychosocial support and patient education is vital in enhancing the quality of life for individuals living with sickle cell anemia. You’ll find that thorough education about your condition empowers you to manage symptoms effectively and make informed decisions about your care.
Studies highlight the importance of ongoing education programs that adapt to the evolving needs of patients at different life stages. These programs reduce hospital readmissions by equipping you with strategies to manage pain and prevent complications at home.
Moreover, psychosocial support addresses the emotional and mental health challenges you may face. The chronic pain associated with sickle cell anemia can lead to psychological stress, including anxiety and depression. Effective support includes counseling, peer support groups, and mental health therapies that are tailored to help you cope with the disease’s impact on your daily life.
Engagement with these support systems has been shown to improve overall mental health and adherence to medical treatments.
Educational and psychosocial interventions are essential. They don’t just help manage the physical symptoms but also improve your ability to engage socially and achieve a better quality of life.
Healthcare Policy and Access to Treatment
As you navigate the complexities of sickle cell anemia, understanding the relationship between insurance coverage and legislative advocacy is essential.
Recent studies have shifted policy frameworks, potentially enhancing your access to emerging treatments and thorough care.
Analyzing these changes, you’ll find insurers are increasingly mandated to cover a broader spectrum of therapeutic options, a direct result of intensified advocacy and updated clinical guidelines.
Insurance Coverage and Legislative Advocacy
Research on sickle cell anemia has greatly impacted insurance coverage and legislative efforts, guaranteeing improved patient access to essential treatments and healthcare services.
- Legislation Enactment: Studies have led to specific laws mandating coverage for thorough sickle cell treatments.
- Insurance Compliance: Enhanced scrutiny guarantees that insurers adhere to these laws, reducing out-of-pocket costs for you.
- Advocacy Influence: Research outcomes shape advocacy strategies, strengthening support for broader coverage initiatives.
Equity in Healthcare Services
Studies on sickle cell anemia have notably advanced equity in healthcare by tailoring patient care to address both common and unique complications of this genetic disorder. These studies have played a vital role in the development of protocols that guarantee you receive a personalized treatment plan, which is essential given the diversity of symptoms among patients. This approach not only enhances the effectiveness of medical interventions but also markedly reduces healthcare disparities experienced by minority groups mostly affected by this condition.
Research has led to the implementation of thorough screening programs that facilitate early diagnosis and management of the disease. Such initiatives ensure that you’re provided with timely and appropriate care, minimizing the risk of severe complications.
Furthermore, these studies have informed the creation of educational resources aimed at healthcare providers to heighten awareness and understanding of the disease’s complexities. This results in a more informed and sensitive approach to your care, reflecting an equitable healthcare system.
Additionally, ongoing research continues to explore novel therapeutic strategies, including gene therapy and new pharmacological treatments, promising to further personalize and improve the quality of care you receive. Each advancement underscores a commitment to reducing health inequities and enhancing life outcomes for individuals with sickle cell anemia.
Future Directions in Sickle Cell Anemia Studies
As you explore the future directions in sickle cell anemia research, you’ll observe a significant shift towards emerging trends that leverage novel therapeutic strategies and advanced genetic editing tools.
You must consider the impact of essential collaborative efforts in data sharing, which are vital for accelerating the pace of discovery and refining treatment protocols.
Lastly, the integration of patient-centered care models promises to tailor treatments to individual patient needs, potentially improving clinical outcomes and quality of life for those affected.
Emerging Trends in Research
As you explore the future of sickle cell anemia research, you’ll find that precision medicine approaches are increasingly central. These strategies involve tailoring treatments based on individual genetic profiles, which could greatly enhance efficacy and reduce adverse effects.
Precision Medicine Approaches
Precision medicine approaches are increasingly transforming the landscape of sickle cell anemia research by tailoring treatments to individual genetic profiles.
Here’s how this impacts you:
- Personalized Therapeutics: Drugs are designed based on your unique genetic makeup, enhancing efficacy and minimizing side effects.
- Gene Editing Techniques: CRISPR technology offers potential cures by directly correcting the genetic defects in your DNA.
- Biomarker Development: Identifies specific markers to predict treatment responses more accurately.
Collaborative Efforts in Data Sharing
Boosting collaborative efforts in data sharing can greatly accelerate the advancement of research in sickle cell anemia. You’re entering an area where vast datasets from diverse genetic populations are essential. Integrating data from various studies enables you to detect patterns and correlations that might otherwise remain obscure. To optimize this, you need robust, interoperable data systems that guarantee data accuracy and accessibility while protecting patient privacy.
In this context, standardizing data formats and establishing common data elements becomes vital. You’ll find it necessary to adopt universally accepted ontologies and metadata standards. This approach not only streamlines data integration and retrieval across multiple platforms but also enhances the reproducibility of research findings.
Consider, too, the role of advanced analytics and machine learning algorithms in mining these extensive datasets. They can provide you with insights into disease mechanisms, potential therapeutic targets, and personalized treatment strategies.
Moreover, fostering global partnerships among research institutions, governments, and international health organizations is essential. These collaborations can facilitate the pooling of resources, expertise, and data, leading to more thorough, cross-population studies. By participating in such networks, you contribute to a collective effort that transcends geographical and disciplinary boundaries, paving the way for groundbreaking discoveries in sickle cell anemia research.
Patient-Centered Care Models
As you explore the future of sickle cell anemia research, it’s imperative to take into account how integrating patient perspectives can transform research design.
By actively involving patients in the development of study protocols, you aren’t only ensuring that the research is more aligned with their needs but also potentially enhancing the applicability and acceptance of clinical outcomes.
This shift toward patient-centered approaches in research necessitates meticulous planning and a deep understanding of patient experiences and expectations.
Incorporating Patient Perspectives in Research Design
Incorporating patient perspectives into research design is vital for developing more effective and empathetic care models in sickle cell anemia studies. Here’s how you can engage:
- Conduct Thorough Interviews:
Gather detailed patient experiences to understand their daily challenges and treatment outcomes.
- Develop Patient Advisory Boards:
Guarantee continuous patient input throughout the research phases.
- Utilize Patient-Reported Outcomes:
Incorporate these metrics to assess treatment efficacy and quality of life improvements.