You might not be aware, but the integration of artificial intelligence (AI) in pediatric anesthesia is changing how you guarantee your child’s safety during medical procedures. By leveraging real-time data and predictive analytics, these systems can now adapt anesthesia delivery to your child’s immediate needs, greatly reducing the risks associated with traditional methods. This shift not only heightens safety but also tailors the anesthesia process to each child’s specific physiological responses. Let’s explore how these innovations not only meet but surpass current safety standards, and consider what this means for the future of pediatric care. Why is this advancement vital for your child’s next procedure?
Pediatric Anesthesia
When addressing pediatric anesthesia, it’s crucial to understand its critical role in ensuring safe surgical procedures for children.
You’ll find that the challenges here are unique, from managing smaller airways to adjusting doses for rapidly changing physiologies.
Additionally, easing a young patient’s anxiety before surgery not only helps them but also supports smoother anesthesia administration and recovery.
Importance of Pediatric Anesthesia
When it comes to pediatric anesthesia, your child’s safety and comfort are paramount.
By tailoring anesthesia techniques specifically for children, healthcare providers can greatly reduce the stress and pain associated with surgical procedures.
This specialized approach not only guarantees a smoother recovery but also minimizes potential risks during and after surgery.
Enhancing Safety and Comfort
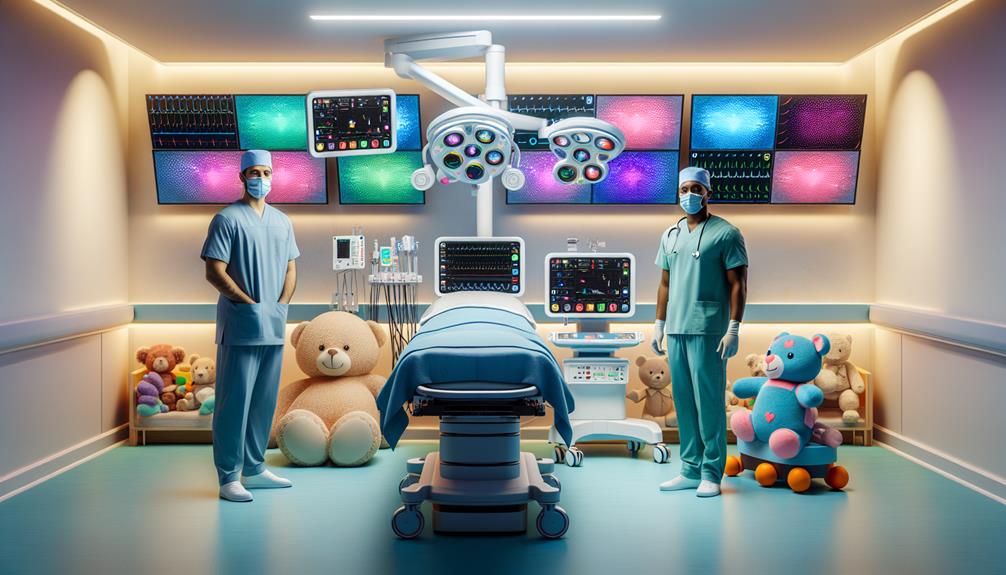
Improving safety and comfort in pediatric anesthesia is essential, as it greatly reduces the risk of complications and eases the stress experienced by young patients and their families.
Tailoring anesthesia methods to each child’s specific needs and continuously monitoring vital signs are critical.
Utilizing child-friendly environments and explanations also helps alleviate fears, ensuring both the physical and emotional well-being of your child during medical procedures.
Challenges in Pediatric Anesthesia
You’ll find that one of the major hurdles in pediatric anesthesia is achieving accurate dosage precision. Children aren’t just small adults; their bodies react to anesthesia in profoundly different ways, making standard dosing formulas less applicable.
It’s important to tailor every anesthetic plan to the individual child’s weight, age, and health condition to guarantee safety and effectiveness.
Addressing Dosage Precision
Achieving precise dosage calculations in pediatric anesthesia is essential, as even small errors can greatly impact a child’s safety and the procedure’s success. You’ll need to carefully evaluate their weight, age, and health conditions meticulously.
Using advanced pharmacokinetic models and real-time monitoring can help guarantee you’re administering the right amount. It’s about combining careful calculation with cutting-edge technology to safeguard these little ones.
Dealing with Pediatric Patients’ Anxiety
Addressing the anxiety of pediatric patients requires a compassionate, tailored approach before administering anesthesia. You’ll find that understanding each child’s fears and providing comfort can greatly ease their preoperative stress. It’s important to establish a trusting relationship early on.
Explain procedures using simple, reassuring language without overwhelming them with details. Small gestures like allowing them to bring a favorite toy or blanket into the pre-op area can make a big difference.
Effective communication extends beyond the child. You’re also tasked with educating the parents about what to expect, which can alleviate their anxiety, indirectly calming the child. Demonstrations of the anesthesia mask with flavored scents can make the experience less intimidating for the child. Remember, a calm parent often means a calm child.
Additionally, incorporating technology like virtual reality headsets to distract during IV placement or anesthesia induction has shown great promise. This tech not only diverts attention but can make the medical environment feel less clinical and more inviting.
Preparation and distraction techniques are essential. They’re not just tools but integral components of pediatric care that ensure the child’s experience is as positive as possible.
Technological Advancements in Pediatric Anesthesia
You’ll find that the introduction of innovative devices for monitoring has greatly enhanced the safety and precision of administering anesthesia to children. These technologies allow for real-time data collection, which is essential in tailoring anesthesia to the specific needs of pediatric patients.
Moreover, automated drug delivery systems offer a level of consistency and accuracy that manual methods can’t match, reducing the risk of human error and improving overall outcomes.
Innovative Devices for Monitoring
As we explore the world of pediatric anesthesia, it’s essential to highlight how innovative monitoring devices are revolutionizing safety and efficacy in treating our youngest patients. You’re likely aware of the inherent challenges pediatric anesthesiologists face, from the anatomical and physiological differences in children to the varied responses they exhibit towards medications and procedures. Modern technology has stepped up, offering tools that not only provide real-time data but also enhance the precision of care delivered.
Here are three groundbreaking devices that have become indispensable in pediatric anesthesia:
- High-Resolution Pulse Oximetry:
This advanced form of pulse oximetry offers more accurate readings of blood oxygen levels, essential for the safe management of anesthesia in children whose oxygenation status can change rapidly.
- Capnography Equipment:
Essential for monitoring carbon dioxide levels, modern capnographs are designed with algorithms to differentiate between adult and pediatric patients, ensuring that the readings are more accurate for the specific respiratory physiology of children.
- Non-Invasive Blood Pressure Monitors:
These devices use sophisticated algorithms to adjust for the smaller arm sizes of children, providing blood pressure readings that are both accurate and less traumatic for the patient.
Each of these tools plays a pivotal role in enhancing the safety protocols necessary during pediatric procedures, ensuring that your child receives the best possible care under anesthesia.
Advantages of Automated Drug Delivery Systems
Automated drug delivery systems in pediatric anesthesia greatly enhance dosing accuracy and patient safety, adapting seamlessly to the unique needs of young patients. These systems meticulously regulate anesthesia delivery, guaranteeing that the exact amount needed is administered based on real-time data, such as weight, age, and medical history. This level of precision reduces the risk of both underdosing and overdosing, which are particularly crucial considerations in such a vulnerable population.
You’ll find these systems equipped with advanced sensors and algorithms that respond dynamically to changes in a child’s vital signs during procedures. This responsiveness ensures that the anesthesia is administered safely and effectively, continuously adjusting to the patient’s needs moment by moment. The automation also frees up healthcare professionals to focus more on other critical aspects of care, rather than manual adjustments and monitoring.
Moreover, automated systems often come with detailed logging capabilities, providing a thorough record of anesthesia management. This is invaluable for post-operative review and future care planning, ensuring any potential issues can be addressed swiftly and thoroughly. By integrating these innovative systems, healthcare settings can greatly enhance the overall safety and efficiency of pediatric anesthesia care, giving you peace of mind that children are receiving the best possible treatment.
Best Practices in Pediatric Anesthesia Management
As you consider the complexities of pediatric anesthesia, it’s essential to embrace a collaborative care approach that involves a team of specialists tailored to each child’s needs.
You’ll need to adjust anesthesia plans according to the diverse age groups you encounter, recognizing the unique physiological responses and developmental considerations of each.
Lastly, don’t underestimate the importance of diligent postoperative monitoring to promptly address any complications and guarantee a smooth recovery for your young patients.
Collaborative Care Approach
In pediatric anesthesia management, adopting a collaborative care approach enhances patient outcomes by integrating the expertise of multidisciplinary teams. You’re not just relying on the anesthesiologist; you’re tapping into a holistic team that includes pediatricians, nurses, and other specialists. This synergy ensures that all aspects of the child’s well-being are considered, making the anesthesia process as safe and effective as possible.
Here’s how you can implement a collaborative care approach effectively:
- Frequent Communication: Make sure that there are open lines of communication among all team members. Regular team meetings and shared platforms for updates can keep everyone informed about the patient’s status and any changes to their care plan.
- Role Clarity: Clearly define each team member’s roles and responsibilities. This clarity prevents overlap and ensures that each aspect of the patient’s care is covered by an appropriate expert.
- Joint Decision-Making: Involve the entire team in the planning and execution of anesthesia plans. This inclusion fosters a deeper understanding and consensus, which is important in managing the nuances of pediatric care.
Tailoring Anesthesia Plans for Different Age Groups
Tailoring anesthesia plans to accommodate the diverse physiological changes observed across different pediatric age groups is essential for their safety and comfort. You’ll find that infants, toddlers, and adolescents don’t just differ in size but also in their metabolic capacities and organ function, which impacts how their bodies handle anesthesia.
For neonates and infants, you must be especially cautious due to their underdeveloped organ systems. They’re more prone to rapid changes in blood pressure, heart rate, and oxygen saturation. Therefore, using lower doses of anesthesia and closely monitoring vital signs is crucial. It’s also important to consider that neonates have a higher body water content, which can affect drug distribution.
As you move to toddlers and young children, their increased curiosity and anxiety about medical environments play a role. Here, using premedication for easing anxiety can be beneficial. These age groups begin to exhibit more robust physiological responses, yet they still require careful dose adjustments and considerations for their still-developing liver and kidney functions.
When dealing with adolescents, remember they’re nearing adult physiological functions but aren’t quite there yet. They might metabolize drugs more quickly than younger children, necessitating adjustments in dosing. Always take into account both their physical and psychological maturity when planning anesthesia.
Importance of Postoperative Monitoring
After carefully planning and administering anesthesia to pediatric patients, it’s equally important to monitor them closely postoperatively to guarantee their safety and comfort. This attentive surveillance plays a pivotal role in swiftly identifying and managing potential complications, ensuring a smoother recovery for your child.
Here are three essential aspects of postoperative monitoring:
- Vital Signs Monitoring: Continuously tracking essential signs—heart rate, blood pressure, oxygen saturation, and respiratory rate—is necessary. Any deviation from normal can be an early indicator of issues like respiratory depression or hemodynamic instability, enabling timely intervention.
- Pain Management: Effective pain control isn’t just about comfort; it’s critical for recovery. Regular assessment using age-appropriate pain scales helps tailor pain management strategies, minimizing distress and facilitating quicker rehabilitation.
- Sedation Level Assessment: Post-anesthesia, children may experience varying levels of sedation. Regularly evaluating their level of consciousness using tools like the Pediatric Sedation State Scale helps prevent complications associated with over-sedation, such as respiratory depression.
Future Trends in Pediatric Anesthesia
As you look ahead, the integration of artificial intelligence in pediatric anesthesia decision-making promises to enhance precision and safety in treatments.
You’ll see how personalized care in anesthesia can be tailored to each child’s specific physiological and genetic profile, optimizing outcomes and minimizing risks.
These advancements are vital in our ongoing effort to improve comfort and efficacy in pediatric anesthesia care.
Integration of Artificial Intelligence in Anesthesia Decision-making
With the integration of artificial intelligence, pediatric anesthesia decision-making is becoming more precise, enhancing safety and outcomes for young patients. You’ll find that AI’s capabilities in analyzing vast datasets far surpass the manual efforts previously employed, leading to more informed and accurate decisions.
Here’s how AI is revolutionizing this critical field:
- Real-Time Monitoring and Adjustments: AI systems can continuously monitor patient vitals and anesthesia levels, making immediate adjustments as needed. This reduces the risk of human error and ensures that the anesthesia is administered at the safest possible levels throughout the procedure.
- Predictive Analytics: AI utilizes historical data and current patient information to predict potential complications before they occur. This proactive approach allows you to anticipate and mitigate risks, rather than merely reacting to them.
- Enhanced Training Tools: Through simulation and virtual reality integrated with AI, you’re able to train in highly realistic scenarios. This not only improves your skills but also prepares you for a wide range of potential situations, enhancing your ability to provide safe and effective care.
AI’s integration into pediatric anesthesia isn’t just about keeping pace with technology—it’s about actively improving the standard of care, ensuring that every child receives the best possible outcome during medical procedures.
Personalized Anesthesia Care for Pediatric Patients
Building on the advancements of AI in pediatric anesthesia, we now see a promising future in tailoring anesthesia care to meet the unique needs of each young patient. By integrating detailed genetic, physiological, and environmental data, personalized anesthesia plans enhance safety and efficacy, ensuring that your child receives the most suitable sedation or pain management.
You’ll find that this approach minimizes risks associated with one-size-fits-all protocols. Imagine a scenario where your child’s medication response is predicted through genetic analysis, allowing anesthesiologists to select agents with fewer side effects and best effectiveness. This isn’t just a distant dream—it’s rapidly becoming a reality with advancements in pharmacogenomics and bioinformatics.
Moreover, personalized care extends beyond drug selection. It includes meticulous preoperative assessments tailored to uncover any potential issues that might influence anesthesia strategies. This means considering everything from past medical history to current emotional state, ensuring that your child is as comfortable and calm as possible throughout the procedure.
With these innovations, anesthesiologists are better equipped to manage the unique challenges presented by pediatric patients, from newborns to teenagers, making anesthesia safer and more effective for every child.
This is the future of pediatric anesthesia: detailed, compassionate, and tailored to each young patient’s specific needs.